The Senior Care Policy Briefing covers important long-term care issues by highlighting policy updates, news reports, and academic research.
Read the full Senior Care Policy Briefing below or download here.
May 30, 2025.
NEWSFLASH
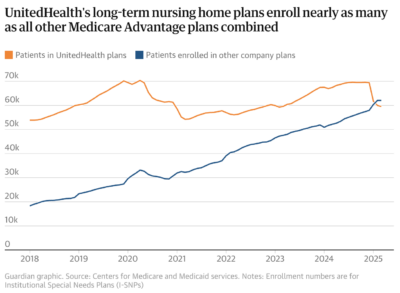
- A recent investigation by The Guardian has uncovered that UnitedHealth Group, the largest U.S. healthcare conglomerate, secretly paid nursing homes bonuses to reduce hospital transfers of residents under its Medicare Advantage plans. The program, aimed at cutting costs, embedded UnitedHealth’s medical staff in nearly 2,000 nursing homes and rewarded facilities with financial incentives for lowering hospital admissions. However, this cost-cutting approach allegedly led to delayed or denied emergency hospital care, resulting in worsening patient outcomes, including permanent brain damage in some cases.
- Internal documents and whistleblower testimony exposed the pressure tactics used on nursing home staff to follow UnitedHealth’s protocols, often overriding medical necessity and personal wishes of patients. Employees faced quotas and tracked metrics like “admits per thousand” to control expenses.
- This investigation raises significant concerns about the ethical implications of profit-driven incentives in elder care and the potential risks to patient safety. It underscores the need for increased transparency and oversight in programs that impact vulnerable populations.
- Is your nursing home affected? You can search for nursing homes that contract with UnitedHealth by visiting: uhcnursinghomeplan.com.
NEW EVIDENCE-BASED METHODOLOGY TO I.D. SUFFICIENT STAFFING
- Chronic understaffing remains a widespread problem in nursing homes, despite federal requirements mandating sufficient staffing to meet residents’ needs.
- The persistence of this problem stems from inadequate oversight and limited public transparency regarding how facilities align staffing with resident care needs.
- A new clinical study, “Nursing Home Guide to Adjusting Nurse Staffing for Resident Case-Mix,” introduces a methodology developed by Robert McLaughlin and Professor Charlene Harrington. This approach calculates expected staffing levels based on each facility’s resident case-mix – the care needs identified in the facility’s own assessments.
- Beginning this month, the Long Term Care Community Coalition (LTCCC) is incorporating these expected staffing levels into its quarterly staffing reports for every U.S. nursing home, using publicly reported federal data.
- Key finding: 90% of nursing homes do not meet the expected staffing thresholds that they are paid to provide based on the needs of their residents (based on the federal staffing report for 2024 Q3).
- As Prof. Harrington noted, “Medicare pays for higher-need residents—but there’s no requirement to actually deliver the care those residents need.”
