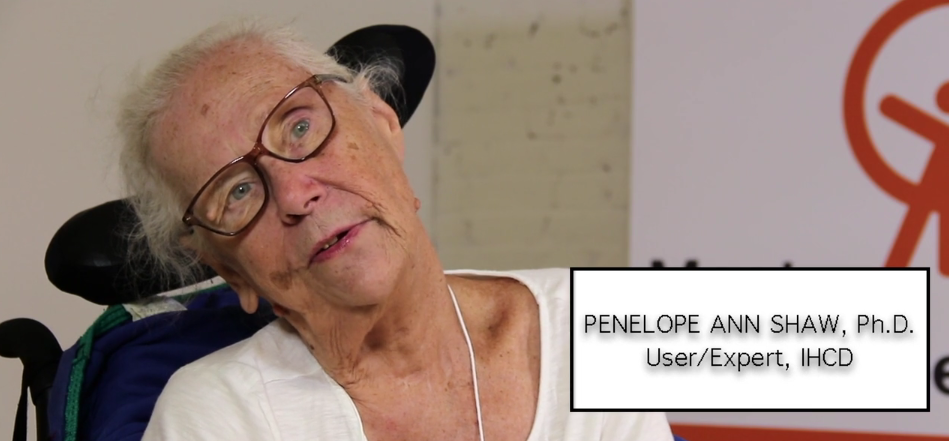
Penny Shaw, Resident and Advocate
Penny Shaw has lived in a nursing home in Massachusetts for nearly two decades and is a renowned advocate for residents in long-term care. Penny is a policy advisor to CMS and was part of the White House’s Coronavirus Commission for Safety and Quality in Nursing Homes. Click the black squares ![]() below to hear and read about Penny’s experience during the COVID-19 pandemic. The expanded interview (edited for clarity) is available at the bottom of the page.
below to hear and read about Penny’s experience during the COVID-19 pandemic. The expanded interview (edited for clarity) is available at the bottom of the page.
Click below for the expanded interview (14:55).
