Happy new year, reader! Thank you for your new or continued support of our mission. This year, we are changing up the quarterly LTC Journal to deliver you more timely information on a monthly basis and to better keep you up to date about what’s happening at NursingHome411! If you haven’t already, be sure to sign up for LTCCC news and alerts.
New at NursingHome411
 A Decade of Drugging
A Decade of Drugging
The Long Term Care Community Coalition published a report, “A Decade of Drugging,” examining how dementia care has – and hasn’t – changed since the launch of the National Partnership to Improve Dementia Care in 2012 by the Centers for Medicare and Medicaid Services (CMS). Based on analysis of public antipsychotic drugging data, academic research, government reports, media investigations, and discussions with long-term care stakeholders including residents, families, ombudsmen, providers, and advocates, we find that a once-promising campaign has sputtered and fallen short of its goals to curb AP drug use.
Read the full report at https://nursinghome411.org/reports/decade-drugs/.
Joint Statement: MACPAC Report Calls for Increased Transparency in Nursing Home Spending
Day after day, the nursing home industry tells residents, families, and our political leaders that Medicaid rates are insufficient to hire more staff or provide better care. The fact is that there is virtually no accountability for where our Medicaid dollars go.
A new report by MACPAC, a non-partisan legislative branch agency, states what resident advocates have been saying for years: we need increased transparency in nursing home finances. The report found that the actual costs of Medicaid in nursing homes could not be calculated because of a lack of transparency in Medicaid spending. As a result, MACPAC could not determine the adequacy of Medicaid payments to nursing homes.
Read the full statement by LTCCC and other advocates at https://nursinghome411.org/macpac-report-transparency/.
Poisoned: Elder Justice “No Harm” Newsletter
In the Elder Justice Newsletter (EJN), we highlight citations, including deficiencies related to abuse, neglect, and substandard care, that have been identified as not causing any resident harm. The newsletter, published jointly with the Center for Medicare Advocacy, sheds light on the issue of so-called “no harm” deficiencies, which typically result in no fine or penalty to the nursing home. Our latest edition of the EJN includes the following “no harm” violations
- Poisoned: Lack of supervision at one-star nursing home leads to resident’s death.
- Moaning and yelling: Resident suffers excessive pain due to poor pain management.
- 91 degrees: One-star nursing home fails to provide safe living environment.
- Unkempt, messy, greasy: A surveyor’s description of unbathed residents.
- Avoidable accident: Resident falls after being left unattended on toilet.
- “Severe sadness”: One-star nursing home fails to provide appropriate medication.
Do these deficiencies sound like “no harm” to you? Check out the full newsletter and previous issues at https://nursinghome411.org/elder-justice.
Food for Thought and More in LTCCC’s Monthly Webinars
LTCCC conducts free monthly Zoom webinars on a variety of timely nursing home topics led by advocates and experts in long-term care. Our December webinar, “Garden of Eatin’,” featured a discussion on resident-directed dining that makes a difference in nursing homes. The program, led by Rebecca Priest (Project Coach, The Green House Project) and Linda McCoy (Dining Practice Partner, St. John’s Home), focused on 24-7 access to food and meals, simplifying menus and providing special experiences, and real food vs. supplements. LTCCC’s webinars are available on our YouTube channel and on the NursingHome411 webinar and events page.
Nursing Homes by the Numbers
Looking for nursing home numbers? Then head to the NursingHome411 Data Center. In December, LTCCC published four new user-friendly nursing home datasets: Staffing, Provider Info, Citations, & Penalties. Whether you’re a consumer, family member, ombudsman, researcher, journalist, policymaker, or advocate, these data can offer valuable information on nursing homes at the provider, state, CMS Region, and national level.
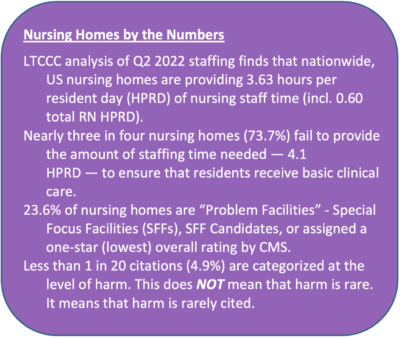
Here’s some more information about the data…
1) Nursing Home Staffing (Q2 2022): This dataset includes staffing levels for every US nursing home, including nurse staffing, contract staffing, and non-nurse staffing. This information is crucial for understanding the quality of care provided by nursing homes and identifying which nursing homes are understaffed. It is based on quarterly payroll-based journal data.
2) Provider Info: This dataset contains facility-level data (five-star ratings, ownership status, health inspection outcomes, etc.) for all US nursing homes. You can also download a “Problem Facilities” dataset which includes only the worst performing nursing homes. This is a useful resource for assessing nursing homes and making informed decisions about where to receive care.
3) Citations: This dataset includes information on citations issued to nursing homes, including the date of the citation, the category of citation (F-tag), and the level of scope and severity. This data is critical for understanding the level of enforcement on nursing homes and identifying whether a nursing home has a history of deficiencies.
4) Penalties: This dataset includes information on fines and payment denials received by nursing homes in the last three years. It is an important tool for assessing the extent to which nursing homes are (or aren’t) held accountable.
We hope these datasets will be useful to you in your research and advocacy efforts. If you have any questions or feedback, please contact us at info@ltccc.org.
Note: These LTCCC datasets are obtained from CMS (https://data.cms.gov/) and reformatted to improve accessibility for consumers. Methodology for LTCCC’s summary findings and other calculations can be found in the “Notes” tabs of the spreadsheets.
The NursingHome411 Podcast: Transfer and Discharge
LTCCC’s “NursingHome411 Podcast” features topical interviews, issue-oriented programming, and audio versions of our webinars. On a recent episode, “Transfer and Discharge,” Lindsay Heckler (Center for Elder Law and Justice) talks all things transfer and discharge: when they’re legal, when they’re illegal, and how to promote safe outcomes for residents. Listen to the NursingHome411 Podcast on our website at https://nursinghome411.org/podcast/, and on Spotify, Apple Podcasts, and Google Podcasts.
Family Council Meetings in the NursingHome411 Zoom Room
LTCCC is pleased to support nursing home family councils and family member settings with our free NursingHome411 Zoom Room. Reserve a room—no time limits!—by visiting bit.ly/fam-council.
Questions about family councils? Learn more at https://nursinghome411.org/families/ or by contacting our Family Empowerment team at families@ltccc.org.

Nursing Home News Highlights
- On the NY minimum staffing mandate … “A 2021 law requires nursing homes to provide 3.5 hours of nursing care per patient day or face daily fines of up to $2,000 daily. It went into effect in December 2022 after being repeatedly delayed due to pandemic conditions and serious labor shortages throughout the state. Although there are no known cases of penalties so far, providers are increasingly worried about the inability to find enough workers to meet the new minimums.” –McKnight’s Long-Term Care News.
- On involuntary transfers… “The Superior Court of the State of California issued a final order January 3, holding that a facility’s refusal to accept a resident back from the hospital “constitutes an involuntary transfer under state and federal law,” and triggers an obligation to follow requirements for discharging a resident.” –AARP.
- On enforcement… “State regulators acknowledged this week that they failed to comply with a law requiring them to triple a fine against an Iowa nursing home where a woman bled to death… Under Iowa law, the director of the Department of Inspections and Appeals is required to triple the penalties against nursing homes for any second or subsequent Class I or Class II violations – which are the most serious type of violations – if they occur within 12 months of the previous violation.” –Iowa Capital Dispatch.
- On understaffing… “The nursing home whose staffing issues during a 2022 winter storm left two patients dead paid thousands in fines… The investigation found that patients were not properly cared for. For over twelve hours, patients starved, sat in their own waste and were not given their necessary medications. The state investigators say that the administrators and leaders at the home failed to properly prepare for the weather and did not notify staff of the emergency preparedness plan.” –Fox 8.
- On oversight… “A Kansas program that awards nursing homes millions of dollars for providing thoughtful care doesn’t weed out those with a history of deficiencies. Critics say it’s just one way the state fails to adequately regulate the long-term care industry.” –NPR.

Nursing Home Research Highlights
- On staff vaccination rates and staffing levels… “Results suggest the federal COVID-19 vaccine mandate has not caused clinically material changes in nursing home’s nurse aide and licensed nurse staffing levels, which continue to be primarily associated with factors that are well-known to researchers and practitioners.” –JAMDA.
- On COVID-19 Boosters… “[A]s newer, more infectious and transmissible variants of the virus emerged, the original 2-dose regimen of the COVID-19 vaccine as recommended in December 2020 was no longer associated with lower rates of adverse COVID-19 outcomes in nursing homes. Policy makers may want to consider longer-term policy options to increase the uptake of booster doses among staff in nursing homes.” –JAMA Network.
- On staying hydrated… “When compared to their well-hydrated peers, participants were more likely to have chronic conditions and show signs of advanced biological aging when their serum sodium levels indicated underhydration. Poorly hydrated adults were also more likely to die at a younger age than their well-hydrated peers, reported the authors, of the National Heart Lung and Blood Institute in Bethesda, MD.” –McKnight’s Long-Term Care News.
- On Alzheimer’s treatments… “The Food and Drug Administration on Friday approved a new Alzheimer’s drugthat may modestly slow the pace of cognitive decline early in the disease, but also carries risks of swelling and bleeding in the brain. The approval of the drug, lecanemab, to be marketed as Leqembi, is likely to generate considerable interest from patients and physicians.” –The New York Times.
- “At the time of the stroke, the patient was participating in a lecanemab trial. The new report confirms the opinion of expert observers on the cause of her death. Blood vessels in the patient’s brain were already likely weakened by lecanemab, they theorized. The stroke drug tPA, an anticoagulant given to some stroke patients, likely further increased the risk of a brain bleed.” –McKnight’s Long-Term Care News.
- On infections and dementia… “These findings bolster support for the hypothesis that infections contribute to the causes of dementia. Furthermore, they highlight that the risk of dementia differs by infection type, suggesting that specific pathophysiological aspects of an infection might affect dementia risk.” –JAMA Network.

LTCCC in the Media
- In an op-ed in the Syracuse Post-Standard, LTCCC’s executive director Richard Mollot wrote, “Substandard nursing home care is not inevitable. It persists because wealthy operators, and their battery of highly paid lobbyists in Albany and Washington, have essentially captured our state government. As a result, day after day, year after year, too many nursing homes escape accountability for substandard care, even when it causes needless suffering and degradation. Even when it results in unnecessary death.”
- A Syracuse.com article on the Bishop Rehabilitation & Nursing Center in Syracuse, NY, cited LTCCC’s 2021 report, Broken Promises, “The government is breaking its promise to ensure that residents are safe and treated with dignity.”
- Before finally closing in August 2022, 109 residents and one staff member died at the Andover nursing facility in New Jersey. “It’s only when harm is identified that there is likely to be any penalty. In states that don’t identify harm, there is virtually no chance they’ll be penalized, and that basically gives facilities the freedom to do whatever they want,” Mollot told com.
- New York Attorney General Letitia James filed a lawsuit against Cold Spring Hills Center for Nursing and Rehabilitation. In her petition, she stated that the nursing home submitted false RN staffing data to CMS and cited to LTCCC’s analysis of CMS’s payroll-based journal data.
- LTCCC is pleased to announce the City & State’s “The Responsible 100” list for 2022 includes LTCCC executive director Richard Mollot. “I was driven to this work by the idea of systemic advocacy for individuals who are vulnerable by leveraging my interest and background in law and policy,” Mollot said. “Over the years, though, I have come to appreciate the value in educating and empowering residents, their families and those who work with them. They can be a very powerful voice at every level for better care and treatment in our nursing homes.