The Senior Care Policy Briefing covers important long-term care issues by highlighting policy updates, news reports, and academic research.
Read the full Senior Care Policy Briefing below or download here.
September 30, 2023.
NEWSFLASH
- Americans give nursing homes a D+ for quality of care, according to a survey from West Health and Gallup. Most respondents expressed discomfort with the idea of living in a nursing home or admitting a relative to one, citing concerns about quality of care, cost, and the potential emotional and mental toll. The survey revealed safety is a significant concern, with only 26% considering nursing homes safe places for older adults.
- Takeaway: Industry lobbyists complain that facilities which don’t comply with safe staffing standards will be at risk for closure. The fact is, more Americans are getting care elsewhere because they are afraid to go to a nursing home, or place someone they love in a situation where they are at risk of abuse and neglect.
- Assisted living communities located close to hospitals tend to rely on emergency departments for non-emergency primary care, leading to disruptive and potentially harmful transfers that increase resident risks and Medicare spending, according to a new study.
LTC BY THE NUMBERS
- Failure to Address. A recent OIG audit found that Georgia could better ensure that nursing homes participating in Medicare or Medicaid programs comply with federal requirements related to life safety, emergency preparedness, and infection control if additional resources were available. The audit revealed a combined 155 deficiencies in these areas at 19 out of 20 nursing homes examined, putting residents, staff, and visitors at greater risk during emergencies or infectious disease outbreaks.
- Over 15,000 Dead. A surge in civil lawsuits related to Covid-19 deaths in New York is targeting not only top state officials but also nursing homes, with families seeking legal recourse. These lawsuits allege negligence by state officials for issuing directives that may have contributed to infections and deaths in nursing homes, and they are raising questions about whether nursing homes have immunity from liability.
GET THE FACTS
- State inspectors, who would enforce the Biden administration’s new nursing home staffing requirements, are facing their own workforce shortages. More than 30 state survey agencies have high vacancy rates, impacting nursing home oversight, and there are concerns about whether these agencies are adequately prepared to enforce the federal staffing requirements effectively.
- Welltower, a real estate investment trust, reported a positive third quarter marked by stronger seniors housing fundamentals. Welltower noted that expenses are stabilizing, and staffing challenges are improving in the senior housing sector.
- Highly paid nursing home lobbyists groan at the mere idea of a safe staffing standard, even one that would only raise overall staff for the bottom 15% of facilities. How many dollars in extra profits is a resident’s life worth?
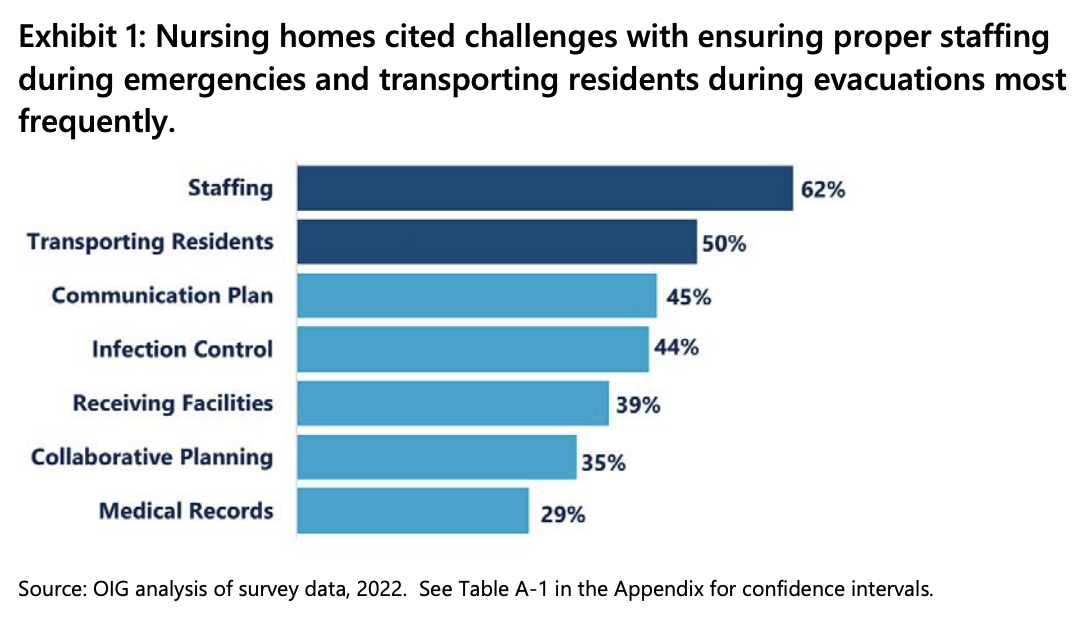
In June 2022, more than three in four nursing homes in disaster-prone areas faced difficulties with emergency preparedness, including with staffing and resident transportation, according to a new report by the Office of Inspector General. Still, less than one-fourth of nursing homes in these high-risk areas received a deficiency for not meeting emergency preparedness requirements. Challenges were more prevalent in nursing homes with lower community resilience, suggesting community resources play a role, and one in five had trouble coordinating with various community partners for preparedness activities.