The Senior Care Policy Briefing covers important long-term care issues by highlighting policy updates, news reports, and academic research.
Read the full Senior Care Policy Briefing below or download here.
October 31, 2024.
Overbilling and Killing? An Examination of the Skilled Nursing Industry is a new study on the extent to which some nursing homes manipulate the reimbursement system to maximize profits and the impact of these practices on both patient safety and the integrity of the use of the public funds which pay for most nursing home care in the United States.
These issues have been top concerns for LTCCC, especially in light of recent studies showing excessive hidden profits and tunneling of profits into related-parties in the nursing home industry. Five years ago, the federal Centers for Medicare & Medicaid Services (CMS) revised its payment system for Medicare services due to concerns about fraud. The new system, the Patient Driven Payment Model (PDPM), was supposed to reduce costs and improve efficiency. Unfortunately, as the authors of this new study found, the revised system is also prone to manipulation by predatory operators. This issue of the Brief is dedicated to some of their key findings.
OVERBILLING AND MASKING POOR CARE
- Some nursing homes, referred to as “opportunistic systems,” systematically overcharge for care, particularly in rehabilitation services, to maximize profits. This overbilling contributes to rising healthcare costs while draining public funds meant for care. It has resulted in overbilling Medicare by an estimated $4.3 billion, while patient outcomes have worsened significantly.
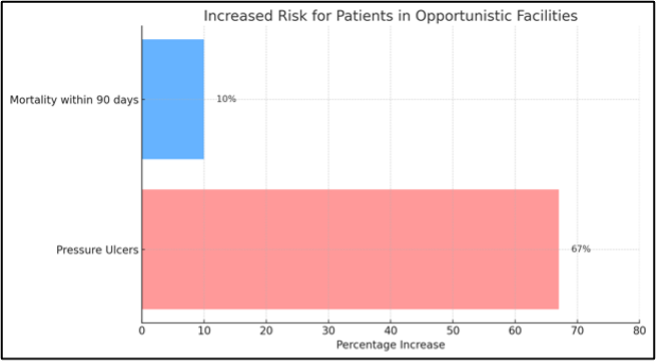
- Patients at these facilities are 67% more likely to develop pressure ulcers and nearly 10% more likely to die within 90 days of leaving the facility.
- The data suggest that this has contributed to an additional 35,000 hospitalizations and 30,000 deaths since PDPM’s implementation in 2019.
- These facilities underreport preventable conditions such as pressure ulcers, urinary tract infections, and traumatic falls, artificially inflating their CMS ratings.
- These deceptive practices mislead residents and families who rely on these ratings to choose providers. In reality, these facilities have lower staffing, more health deficiencies, and twice as many substantiated complaints as their more ethical counterparts.
CORPORATE GREED AND EXPANSION
- Many of these operators cut costs by reducing nurse staffing, providing 37% fewer registered nurse hours compared to other facilities.
- In the worst-offending facilities, 38.7% of patients were receiving the most intensive rehab care right up to the day of their death – indicating a focus on maximizing revenue rather than providing appropriate care.
CONCLUSION AND A CALL FOR REFORM
- “First, the fact that SNF systems have such widespread and persistent differences in fraud and health outcomes indicates that better care at lower prices is feasible….”
- “Second, given that existing methods of reporting preventable health outcomes are gamed, much more attention needs to be spent on measuring and quantifying patient health outcomes.”
- “Third, enforcement penalties need to be substantially increased.”
