President Biden has promised to reform nursing homes by setting a national minimum staffing standard. Unfortunately, the proposed rule is woefully inadequate to meet residents’ needs. LTCCC submitted the below comments, and although the public comment period concluded, there’s still time to make your voice heard.
Please consider sharing your comments with your Senators and Member of Congress by using our Action Alert. Your federal representatives have a lot of influence on this process. You can write your own message or use our provided template. The message will be automatically sent to your federal representatives. Click here to contact your federal representatives.
November 6, 2023
Administrator Chiquita Brooks-LaSure
Centers for Medicare & Medicaid Services
Department of Health and Human Services
Attention: CMS-3442-P
P.O. Box 8016
Baltimore, MD 21244-8016
Re: CMS-3442-P; Medicare and Medicaid Programs; Minimum Staffing Standards for Long-Term Care Facilities and Medicaid Institutional Payment Transparency Reporting
Submitted electronically: www.regulations.gov
Dear Administrator Brooks-LaSure and CMS Colleagues:
The Long Term Care Community Coalition (LTCCC) is a national non-profit organization dedicated to improving care, quality of life, and dignity for residents in nursing homes and other long-term residential care settings. For over 30 years, LTCCC has conducted policy studies and quantitative analyses of nursing home laws, standards, and their implementation. In addition to its work on systemic nursing home issues, LTCCC works closely with residents, families, and their advocates to improve care.
We respectfully submit the following comments in response to CMS’s proposed rule that would establish minimum staffing standards for long-term care facilities and require states to report the percent of Medicaid payments for certain Medicaid-covered institutional services that are spent on compensation for direct care workers and support staff. In addition to our comments, LTCCC supports those of the Geriatric Circle (Charlene Harrington, et al.).
I. Introduction and Foundation for Our Comments
Staffing levels are a critical indicator of a nursing home’s quality and safety. Decades of research shows that nursing homes with more nursing staff have better quality, on-site survey scores, and resident outcome measures.[1] [2] Conversely, residents in understaffed nursing homes are more likely to suffer harm, live in degrading conditions, and experience negative outcomes.[3] Nevertheless, understaffing is a widespread and persistent problem in nursing homes nationwide. This understaffing has serious repercussions for residents and direct care staff. Despite the billions of dollars we invest in nursing home care every year, significant problems in resident care, quality of life, and dignity are pervasive across the country.
The COVID-19 pandemic further demonstrated the need for adequate staffing in nursing homes, with numerous studies and reports linking higher direct care staffing levels to fewer COVID-19 outbreaks and resident deaths.[4] [5] [6]
For several decades, minimum staffing requirements have been the subject of extensive debate at both the federal and state levels. In 1987, in response to media and government reports shining light on the deplorable state of nursing home care, Congress passed the Nursing Home Reform Law of 1987.[7] The extensive reforms in the Reform Law included basic requirements for nurse staffing that remain in place today. Those standards, however, are extremely limited, and in some instances, vague and subjective.
Currently, to ensure that residents receive good care and are safe, the federal nursing home requirements mandate that facilities “have sufficient nursing staff with the appropriate competencies and skills sets to provide nursing and related services to assure resident safety and attain or maintain the highest practicable physical, mental, and psychosocial well-being of each resident, as determined by resident assessments and individual plans of care and considering the number, acuity and diagnoses of the facility’s resident population in accordance with the facility assessment required at §483.70(e).”[8]
Many nursing homes take the current law, and their duty to their residents and communities seriously. Unfortunately, in the absence of meaningful enforcement, too many nursing homes understaff and flout minimum standards with impunity. Implementing a minimum staffing standard will directly impact the quality of care provided to some of society’s most vulnerable individuals. However, CMS’s current proposed minimum staffing levels are far too low. An analysis of federal nursing home staffing data shows that U.S. nursing homes provided 3.63 total staff HPRD (hours per resident day) in the first quarter of 2023. This is well above CMS’s proposed minimum of 3.0 HPRD, but far below the 4.1 HPRD residents require for their clinical care needs to be met. CMS’s own 2001 report[9] and decades of subsequent research on the minimum staffing necessary to provide a safe and humane environment for both residents and staff support a minimum standard of at least 4.1 total nursing HPRD. LTCCC strongly encourages CMS to establish a higher mandatory minimum staffing standard, with 4.1 HPRD as the starting point.
II. The 2023 Abt Nurse Staffing Study Is Limited and Inadequate
In February 2022, the Biden Administration announced it would propose new regulations establishing more specific, detailed, and quantitative minimum staffing requirements by Spring 2023. President Biden’s announcement cited adequate staffing levels as the “measure most closely linked to the quality of care residents receive.”[10] To inform the rulemaking, CMS issued a Request for Information that received thousands of comments. Unfortunately, based on the current proposal, it seems as though CMS ignored the comments of long-term care experts and resident advocates as well as the experiences of nursing home residents.
CMS also conducted a staffing study[11] to help identify a minimum staffing level, or “threshold below which residents would be at substantially increased risk of not receiving the safe and quality care they deserve.”[12] However, CMS did not conduct an evidence-based analysis determining the time needed to provide care to nursing home residents in accordance with the requirements laid out in the 1987 Nursing Home Reform Law. As a result, the study which CMS conducted to support development of a rule was significantly flawed and limited. While the study begins by pointing out the seminal 2001 CMS report to Congress on the appropriateness of minimum staffing standards,[13] it omits a crucial point that total nurse staffing for nursing home residents of below 4.1 HPRD, with .55 (for short stay and .75 RN staffing for long stay residents), .55 LPN staffing, and 2.4 to 2.8 CNA HPRD led to a likelihood of harm or jeopardy to residents. Because those findings are over 20 years old, CMS should have focused on whether the extent to which they are still valid and might need to be updated to reflect (among other factors) the extent to which resident acuity has increased over the last 22 years.
Furthermore, the simulation study only modeled five licensed nursing tasks, and failed to consider the amount of time that nurses must spend on interrupted care because of urgent unplanned care needed by residents. Furthermore, CMS did not address or provide time to ensure that residents are treated humanely and with dignity, and that there is time to implement essential non-clinical tasks, including effective infection control protocols, as long required by the Nursing Home Reform Law. This is unacceptable. As stated above, CMS’s own 2001 study, and numerous other studies, established the importance of having a minimum of 4.1 HPRD just to meet basic clinical needs. Surely, after the nation witnessed the emotional and psycho-social toll inflicted on so many residents during the pandemic (which, to a large extent, continues to this day), it is incumbent upon CMS to promulgate a standard that ensures not only clinical well-being, but freedom from degradation and inhumane conditions, too.
LTCCC calls on CMS to undertake a new, evidence-based study determining the amount of time needed to provide clinical care and other non-clinical services to residents with different levels of need ensuring a standard that upholds residents’ dignity and humane treatment. CMS should establish a set time frame, with a maximum of two years, to conduct the study and begin implementing its findings.
III. The Importance of a Minimum Staffing Standard
CMS’s own 2001 study and numerous studies conducted since 2001 have shown that residents need at least 4.1 HPRD of nursing time just to meet basic clinical needs. Because of the increased acuity of nursing home residents since 2001, 4.1 HPRD must be the starting point for acceptable nursing home care, and the 4.1 HPRD minimum should include at least .75 HPRD of a registered nurse’s time.
a. 24-Hour Registered Nurses Are Critical for Quality Care
Registered n serve a critical role in every nursing home staff. They provide expertise – infection control planning and management, resident assessment and care planning, and the identification and treatment of chronic and acute conditions – to help ensure the clinical, emotional, and psychosocial needs of every resident are being met. CMS itself noted that research suggests that greater RN presence has been associated with higher quality of care and fewer deficiencies.
By definition, nursing home residents need 24/7 skilled nursing. The recommendation for 24-hour registered nurses in nursing homes is one that has been strongly supported by experts for years.[14] Good facilities already provide this level of staffing or more. The time has come to ensure that all nursing homes provide this level of care and competency.
CMS proposes revising § 483.35(b)(1) to “require LTC facilities to have an RN onsite 24 hours a day, 7 days a week.” While LTCCC strongly supports the requirement that every facility provide an RN 24 hours a day, seven days a week, it is crucial that the RN be in the building and providing direct care to residents, not merely at a different location or on-call or performing solely administrative duties. Being available is not an acceptable alternative to being in the facility and providing direct care. The 24-hour RN requirement should be modified to require at least one RN per 100 residents 24 hours per day. Otherwise, residents in larger facilities will not have access to vital RN monitoring and care. In addition, LTCCC recommends that director of nursing hours only count toward the 24-hour RN requirement for facilities with
LTCCC also strongly opposes any waiver provisions for RN staffing. CMS’s current proposed waivers and dangerous to the health and safety of residents. If a nursing home is unable to adequately staff with a 24-hour RN for every 100 residents, the nursing home must be required to not admit new residents.
i. CMS and Industry Cost Estimates for 24-Hour RNs Are Inaccurate
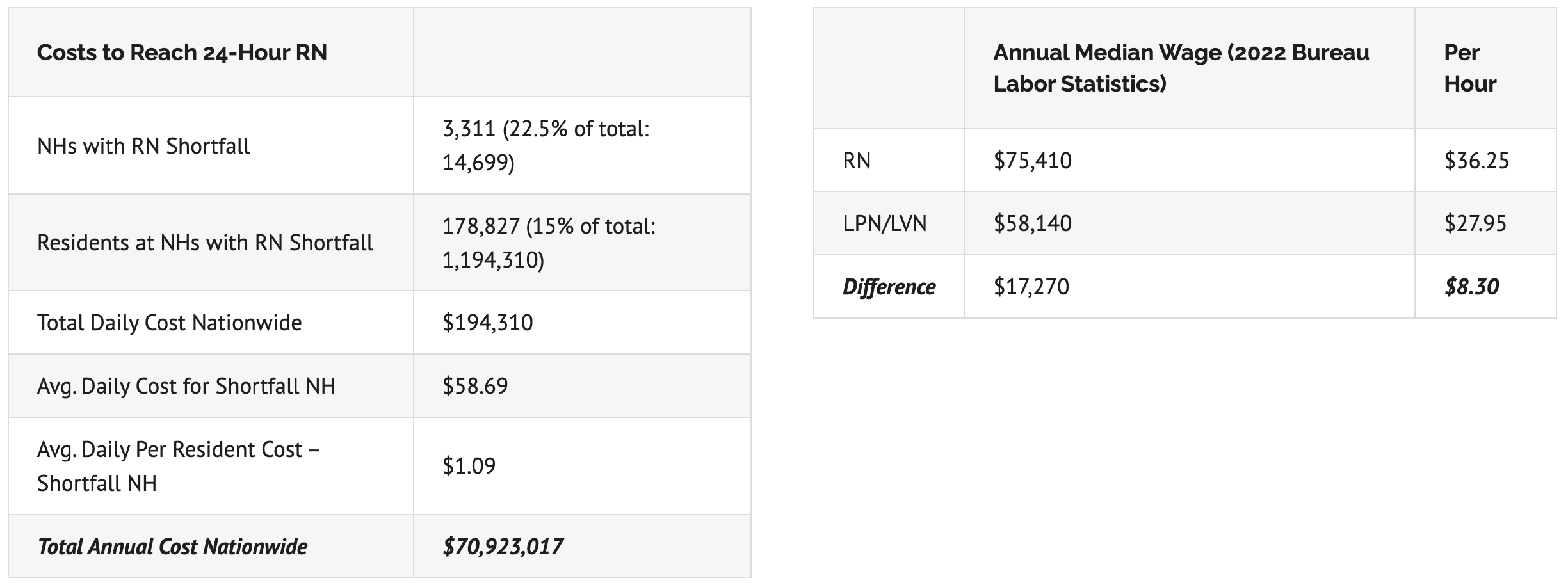
Nursing home industry leaders are claiming it would cost $610 million annually to meet the proposed standard of a 24-hour RN. In fact, the data that nursing homes themselves report to the government indicate that this claim is false, and that the actual costs would be a small fraction of that number. LTCCC conducted an analysis[15] showing that the annual cost of meeting the 24-hour RN staffing standard is only $71 million – just $1.09 per resident per day for facilities with 24-hour RN shortfalls. Our findings are based on government staffing data (reported by facilities) and nursing home staff salary data from the U.S. Department of Labor.
CMS’s proposal assumed that nursing homes would keep their existing LPN staff and hire additional RNs. The fact is that facilities with less than 24-hour RN staffing do not need to hire a bunch of RNs. They can simply shift from LPNs to RNs to bridge the hours needed to cover the gap. This is precisely what the industry did in 2019, when it fired thousands of therapists after CMS changed its methodology for paying for rehabilitation care.
See charts below from LTCCC’s 24-hour RN analysis.
b. Certified Nurse Aides Are Overworked and Underpaid
The evidence suggests that staffing standards work! Researchers have found that specific minimum staffing standards are associated with improvements in staffing, particularly for certified nurse aides (CNAs). CNAs perform the bulk of care received by nursing home residents, but often are burnt out due to the significant understaffing in nursing homes. This burnout in direct care workers leads to worse care for nursing home residents. In addition, nursing assistant wages in nursing homes are lower than wages in hospitals and in comparable entry level jobs for retail salespersons and customer service representatives. Nursing assistants often do not have health insurance and require some form of public assistance. Nursing homes must offer wages that are competitive with jobs that require comparable skills and living wages.
In California and Ohio, the implementation of minimum staffing requirements coincided with a five percent increase in overall HPRD. Though the regulations unintentionally resulted in a reduction in skill mix (i.e., the ratio of RNs to all direct care staff), the staffing requirements led to a decrease in severe deficiency citations and improvement in specific health conditions requiring intensive nursing care.[16] In another study, facilities that served a higher share of Medicaid residents reported larger increases in staffing levels, including RN staffing, as a result of the imposition of minimum staffing requirements. This resulted in larger gains in other measures of quality of care.[17]
LTCCC recommends that CMS adopt a minimum standard of at least 2.8 HPRD for CNAs, a number based on scientific research and expert opinion. CMS’s proposed standard of 2.45 CNA HPRD is totally unacceptable. In addition to staffing at an appropriate level, nursing homes must also be required to pay CNAs a living wage.
i. CMS Cost Estimates for 2.45 NA HPRD Are Inaccurate
CMS’s proposal incorrectly assumed that all nursing homes would retain existing staff and add new CNAs. Without establishing minimum standards for LPNs, nursing homes will likely meet positional requirements by replacing LPNs with other staff. Replacing LPNs with less expensive CNAs would result in estimated hourly savings of $14. Furthermore, replacing LPNs with RNs would increase hourly costs by only $9, a fraction of the cost of hiring a new RN without reducing LPN staff.[18]
c. Total Nurse Staffing Standard
i. Utilizing a Diverse Nursing Skill Mix is Essential
LTCCC supports a nurse staffing requirement that includes RNs, LPNs, and CNAs. Because each type of nursing staff uniquely contributes to resident care, using a nursing skill mix consisting of registered nurses (RNs), licensed vocational/practical nurses (LVN/LPNs), and certified nursing assistants (CNAs) is essential. Different patient needs require a range of skills. Thus, a skill mix enables a more comprehensive approach to care, allowing each nursing professional to work within their scope of practice, enhancing patient outcomes by addressing a variety of health issues.
Under the current proposed rule, there is nothing stopping nursing homes from staffing at exactly 3.0 HPRD. This would be severely detrimental to residents and staff. Furthermore, excluding LPNs from the requirement could lead to nursing homes staffing at .55 RN, as proposed, and filling the rest of the requirement with CNAs. This would result in a lower skill mix and significantly lower staffing overall for the majority of nursing homes.[19]
Though LPNs are not a substitute for RNs, they play a crucial role in nursing homes due to their diverse skill set and contributions to patient care. LPNs often act as a bridge between RNs and CNAs, supporting both, and undertaking many tasks such as administering medications and treatments, monitoring residents’ vital signs, and supporting resident care plans. LPN’s hands-on role in resident care, combined with their medical knowledge and training, makes them an invaluable asset in nursing homes. Therefore, LTCCC urges CMS to incorporate the findings from its own 2001 study[20] to include a minimum LPN/LVN staffing level.
ii. 3.48 HPRD is Woefully Insufficient
CMS’s proposed regulations state it would consider a minimum total nurse staffing standard of 3.48 HPRD, rather than the 3.0 HPRD. Although better than 3.0 HPRD, 3.48 HPRD is still woefully insufficient, and there is no clinical evidence that supports 3.48 HPRD as adequate to maintain resident safety and health. It is well below an acceptable standard of care even for residents with the least needs. It is, fundamentally, an arbitrary and capricious figure that has nothing to do with ensuring that residents receive the care to which they are entitled under the Nursing Home Reform Law and implementing regulations.
iii. 4.1 HPRD Must Be the Starting Point
An acceptable starting point for a minimum staffing standard must begin at 4.1 HPRD, and it must include 0.75 HPRD of a registered nurse’s time. Furthermore, a minimum requirement of 4.1 total nursing hours per resident day, including 0.75 RN hours, 1.4 licensed nursing hours, and 2.8 CNA hours, is financially viable. According to a recent industry study,[21] in 2019, 25% of nursing homes met the minimum 4.1 total nursing HPRD, while 31%, 85%, and 11% met the RN, LPN, and CNA thresholds, respectively. To implement a 4.1 HPRD minimum standard across nursing homes nationwide, the study estimated that an additional annual cost of $7.25 billion is anticipated. Even if one accepts the industry’s numbers, this only accounts for 4.2% of the total national spending on nursing homes, equating to roughly $16 per resident per day.
IV. Waivers and Hardship Exemptions
LTCCC strongly and adamantly opposes providing facilities with waivers for failing to comply with any of the requirements. If a facility falls below the minimum standard, CMS must issue a ban on payments for new admissions. The facility’s ban on payments for new admissions should not be lifted until the facility has documented that it is meeting the standard. In addition, nursing homes should not be allowed to discharge residents to meet the staffing standard without state oversight. A nursing home should not be run like a warehouse for vulnerable elderly and disabled individuals. CMS’s proposed waivers are dangerous for residents.
We find it difficult to understand why CMS would promulgate a hardship exemption that will impose significant hardships on residents. If a facility cannot hire or retain sufficient staff, then it should not be paid for any new admissions. Why would the federal government allow nursing homes to accept or retain residents for whom they clearly do not have sufficient staff to even meet basic needs? Furthermore, if CMS permits exceptions, it sends a message to the industry that facilities can continue to take in and profit from vulnerable residents when they have insufficient staff with impunity. CMS must stop putting the financial priorities of the nursing home industry above the basic needs and dignity of nursing home residents.
a. Rural Area Staffing
People living in rural areas have the same needs as those in urban and suburban areas, despite the differences in their geographical settings. They, too, deserve not to be warehoused in facilities where they will be exposed to greater risk of pressure ulcers, antipsychotic drugging, and other adverse events as well as demeaning and potentially dangerous conditions. In some cases, rural nursing home residents may be more isolated from family and support networks, making the role of the nursing home staff even more crucial in providing social interaction and emotional support. Persistent inadequate staffing levels and considerable variations in nurse-to-resident ratios among different facilities and states heighten the risk of residents receiving substandard and unsafe care, especially in times of public health emergencies. Furthermore, contrary to what the industry says, there is little evidence to support the contention that the staffing crisis is more predominant in rural areas.
V. Implementation of Minimum Staffing Standards
CMS’s proposed implementation time frame for the new requirements is wholly inappropriate, especially given the inadequacy of the proposed staffing levels. All facilities should be given a maximum of two years to meet the staffing standard.
Furthermore, it is unacceptable to provide special delays for rural facilities. Nursing home residents in rural communities are entitled to the same quality and safety as those in urban and suburban areas. Under the current CMS proposal, nursing home residents in rural areas are six to seven years away from what CMS considers “safe staffing.” There should be no delayed implementation of the staffing standard for nursing homes in rural areas.
Given the fact that the average facility has over 50% turnover per year, just by improving working conditions and retention we believe that most if not all facilities could easily achieve a reasonable staffing standard (i.e., one that is at least 4.1 HPRD), no matter the inadequate and arbitrary standard proposed by CMS. Those who cannot achieve the standard within two years must, as a minimum, stop accepting new residents. As noted earlier, nursing homes are not supposed to be operated like a warehouse for vulnerable elderly and disabled individuals.
VI. CMS Should Use PBJ Data to Determine Daily Compliance and Implement Automatic Mandatory Enforcement
Compliance with the minimum nursing staff requirements should be determined using payroll based journal (PBJ) staffing data, similar to the system in place in New York State.[23] Compliance should be carried out electronically with mandatory automatic and substantial penalties imposed for noncompliance. Automatic denial of payment for new admissions should also be used for any substantive non-compliance as well as citations at the resident harm level. There is no reason that CMS should wait for annual surveys to undertake enforcement. Given especially the significant backlog of surveys, this plan is not acceptable.[24]
a. CMS Must Strengthen State Survey Enforcement
Nursing homes too often have inadequate care staff and fail to provide appropriate care with dignity because nothing is stopping them from doing otherwise. Though long recognized as one of the most serious and widespread problems in the nursing home sector, sufficient staffing is rarely cited. Nationwide, sufficient staffing citations totaled just 2,625 in the three-year period from 2018-2020.[25] As data continuously indicate, the government is breaking its promise to ensure that residents are safe and treated with dignity every day. Our studies of national citation data persistently indicate that approximately 95% of nursing home health deficiencies are classified as “not causing harm.”[26] As a result, there is generally little or no punishment when nursing homes fail to provide care that meets the standards they are paid to achieve, even when such failures result in significant resident suffering or avoidable death.[27]
Furthermore, even when staffing deficiencies are appropriately cited, nursing homes are generally provided with an opportunity to correct them, without incurring fines or other penalties. Meanwhile, enforcement action is taken only in about half of the cases of the more serious deficiencies (those CMS identifies as causing “actual harm” or posing “immediate jeopardy).[28] The failure to penalize facilities for inadequate staffing practices – even when they lead to unnecessary suffering or death – sends a perverse message to the nursing home industry: substandard care can be provided to vulnerable individuals with impunity.
The systemic acceptance of subpar care does not only perpetuate resident neglect and abuse; it has a significant financial cost. U.S. taxpayers pay for the majority of nursing home care. We rely on CMS and State Survey Agencies to assure that public monies are spent appropriately. When care is poor it means we are not getting good value for the money we spend. And when that poor care results in the need for additional care, whether it be medication to fight an unnecessary infection or hospitalization due to a medication error, the public generally foots the bill for that, too.
VII. Staffing Supply and Access to Quality Care
The whole point of President Biden’s promise to reform nursing homes is that access to poor care, including situations that are likely to result in neglect or abuse, is not care. Hundreds of thousands of nursing home residents are now suffering every day in facilities with woefully inadequate staffing to meet basic needs, no matter provide treatment with dignity. Thus, it is essential that the federal staffing standard is predicated on the time needed to care for residents safely and with dignity, not bent to accommodate the unsubstantiated claims of low funding and hiring challenges that have been perpetrated by sophisticated operators and their powerful lobby associations for decades.
a. The Problem is Not the Funding
Understaffing, unfortunately, is a common practice among nursing homes striving to reduce operating costs and maximize profits, since personnel expenditures can constitute more than half of operating costs. Though nursing home industry lobbyists have long argued that inadequate staffing is due to insufficient funding, there are no independent, reliable data to support that claim. The fact is that nursing homes are seen as an attractive investment by knowledgeable investors, including real estate investment trusts, private equity firms, and other sophisticated enterprises. Understaffing is particularly common in facilities taken over by private equity firms that aim to rapidly maximize profits.[29] Importantly, a 2014 federal study[30] found that an astonishing one-third of the people who go to nursing homes for Medicare rehab services (which even nursing homes acknowledge are highly profitable) are harmed within an average of 15.5 days after entering the facility. That study found that 59% of the time that harm is “clearly or likely preventable.” In short, reimbursement rates are not an accurate (or appropriate) excuse for insufficient staffing.
The problem is not the amount of funds that nursing homes are paid but, rather, how these funds are being used. Studies have found that, rather than spending on resident care, too many nursing homes are devoting resources for items such as exorbitant administrative costs, unchecked related-party transactions, and excess profits.[31]
b. CMS Must Break the Vicious Cycle of Understaffing
Staffing challenges, while exacerbated during the pandemic, have long plagued the nursing home industry. The industry complains that chronic understaffing could lead to closures. In reality, the reasons for nursing homes’ inability to recruit and retain a sufficient workforce are numerous, multidimensional, and interrelated. They include poor pay and benefits, unrealistic workloads, dangerous working conditions, limited advancement opportunities, and lack of respect.[32] For the most part, the industry has failed to address these persistent problems, instead advocating almost exclusively, for many decades, for funding increases with little to no accountability for that funding. In addition to a long history of opposing minimum staffing ratios that could address the workload issues and rejecting robust minimum training requirements that could improve worker safety, the industry continues to advance failed, band-aid policies that have been proven to exacerbate the staffing problem. We fear that the proposed standard reflects these perspectives and priorities.
Staffing supply issues are the result of high turnover rates, which continue to be a major problem for many of the nation’s nursing homes. The average nursing home turns over more than half (52.9%) of its nursing staff within a year, according to the latest federal data.[33] Turnover rates are to a large extent the result of chronic, widespread understaffing which leads to unreasonable workloads.[34] CNAs are forced to take on unreasonably heavy workloads and become burnt out, leading to high CNA turnover rates (frequently exceeding 100 percent).[35] Recent research has linked higher levels of CNA HPRD to greater CNA retention.[36]
VIII. The Public Deserves Better Nursing Home Transparency
The Reform Law of 1987 set forth the most extensive set of changes to occur in federal nursing home regulation since the passage of Medicaid and Medicare more than two decades earlier. Among its many significant provisions was the public disclosure of information related to annual facility cost reports and statements of ownership and control interest.[37] Despite the positive steps taken in the Reform Law to improve transparency, detailed information about a nursing home’s ownership and finances was for the most part considered confidential and unavailable to regulators or to the public.
Because of lax oversight, many nursing home owners and operators have become increasingly sophisticated in using taxpayer dollars to benefit themselves rather than those for whom these funds are intended – their residents. The millions of dollars of Medicare and Medicaid funds (including COVID-19 related funds) operators receive to care for nursing home residents are, too often, diverted away from resident care and towards items such as bloated administrative salaries, capital expenditures, and other unrelated expenses. Public funds that are paid to operators for resident care often find their way into the coffers of companies owned or controlled by these operators with no practical accountability for the reasonableness of those expenses.
The complexity of ownership and management structures hampers the ability of regulators to effectively monitor how taxpayer dollars are being spent and to ascertain a nursing home’s financial health. While steps have been taken to improve nursing home cost reporting, more needs to be done. Greater transparency of ownership, management, and financial data, combined with sufficient oversight and enforcement authority and the necessary funding to effectively carry out these activities are critically needed.
a. Medicaid Transparency
LTCCC strongly supports increased Medicaid payment transparency requirements. Medicaid is the primary source of funding for nursing home services in the US. Nursing home providers and trade associations incessantly claim that Medicaid reimbursement rates are inadequate and less than the cost of actual care. In fact, the for-profit sector of the industry has been steadily growing for years, indicating that nursing home operators are making profits off of resident care while routinely maintaining low levels of staffing.[38] [39]
In an aim to improve transparency in Medicaid payment data, CMS proposes new regulations that would require State Medicaid agencies report on the percent of payments for Medicaid-covered services in nursing facilities and intermediate care facilities for individuals with intellectual disabilities (ICF/IIDs) that are spent on compensation for the direct care and support staff workforce. While some states have Medicaid wage data available, many lack the comprehensive financial reporting systems to provide detailed compensation information. Further development of those systems would be necessary for most state Medicaid programs to achieve this.
LTCCC encourages CMS to adopt the Medicaid Transparency Recommendations by MACPAC in its recent report, “Principles for Assessing Medicaid Nursing Facility Payment Policies, Chapter 2.”[40] The MACPAC recommendations call for state Medicaid programs to make nursing home payment and cost data publicly available in a standard format and include:
- Base Medicaid payments, supplemental payments, managed care directed payments, and beneficiary contributions to their share of costs.
- The amount of provider contributions to the non-federal share of Medicaid payments to calculate net payments to providers.
- Expenses for wages and benefits separately for nursing, ancillary, and support services as well as administrative staff and other employees.
- Expenses for direct care including staffing costs for nursing, ancillary, and support services.
- Expenses for administration, property, and profits.
- Detailed expenses for related-party transactions, real estate ownership, and disallowed costs.
Although CMS’s proposed regulations do not include changes to improve Medicare financial transparency and accountability, LTCCC supports extending the Medicaid requirements to Medicare expenditures as well, as Medicare is the second largest payor for nursing facility residents, spending about $28.5 billion in nursing homes in 2021.[41]
In 2011, CMS implemented new Medicare cost reporting requirements for skilled nursing homes to collect detailed data on direct care expenditures by category. However, CMS has not yet developed a plan to report these data in a user-friendly format to policymakers and the public, as required by ACA’s Section 6104. Furthermore, cost report data are seldom audited, and penalties are not issued for failure to report.[42] Additionally, nursing home owners and operators can easily manipulate cost reports to conceal profits. Though expenditure data in the cost reports are available to the public, experts describe them as inaccurate and incomplete. Standardized reporting requirements is crucial to establishing transparency, and CMS has the authority under ACA Section 6104 to require reporting on Medicare expenditures for staff compensation. CMS must implement the disclosure and reporting requirement of Section 6104 to both Medicaid and Medicare expenditures.
c. CMS Should Set a Minimum Direct Spending Requirement for All Payers Including Medicare and Medicaid
Until recently, nursing homes have not been required to spend a set minimum percentage of the funds they receive on the care of their residents, nor have the public or policymakers had an effective tool to require accountability for these expenditures. In May 2020, as the number of COVID-19 deaths continued to mount in New Jersey, that state enlisted the Manatt Health consulting firm to make a series of substantive recommendations for reforming its troubled nursing home industry during the pandemic and beyond. One of the recommendations, designed to address both the lack of transparency on how taxpayer funds are spent, as well as the need to require that the bulk of funds be spent on resident care, called for the establishment of a nursing home direct care ratio reporting and rebate requirement.[43]
In September 2020, the New Jersey Legislature passed, and the Governor signed legislation establishing a direct care ratio requirement for nursing homes. The direct care ratio requires that 90 percent of a facility’s aggregate revenue in each fiscal year is to be expended on the direct care of residents, and facilities that fail to meet the direct care ratio will be required to pay a rebate to the state. Three other states[44] (Massachusetts, New York, and Pennsylvania) have also passed legislation requiring a percentage of nursing home revenues to be spent on direct care services.
LTCCC strongly urges CMS to adopt a requirement that nursing homes spend at least 90 percent of revenues on direct care services, as required in New Jersey.[45]
IX. Conclusion
Chronic understaffing has been a longstanding and grim reality for U.S. nursing homes. The failure to provide sufficient staffing has resulted in untold misery and suffering for residents, their families, and nursing staff alike. While the causes of understaffing are complex and multifactorial, experts agree that the lack of clear, sufficient, and enforced minimum staffing requirements is paramount.
Researchers, resident advocates, nurses, and direct care workers have for years been recommending evidence-based policies designed to improve staffing levels in nursing. These include mandated minimum staffing standards; strong and comprehensive training requirements; better, full-time jobs; improved wages, benefits, and empowerment practices for direct care workers; carefully targeted Medicaid payment policies closely tied to improved compensation and staffing improvements; and effective and appropriately funded oversight and enforcement activities (including imposition of meaningful penalties for facilities that fail to meet minimum standards).
Most of these policies, however, have been opposed by a nursing home industry pushing for the same, tired approaches that have long and unsuccessful track records. These band-aid solutions involve seeking greater funding with little to no accountability – eliminating or reducing standards while ultimately weakening oversight and enforcement.
The time is now to move away from overly modest and piecemeal approaches (that have had, at best, only temporary positive results) and implement a policy that truly meets the needs of residents. After more than five decades of failed approaches and insufficient levels of nursing care, nursing home residents, their loved ones, dedicated staff, and the taxpaying deserve no less.
The proposed 3.0 minimum sets a bar far too low for the over 15,000 US nursing homes. Accepting this standard is accepting a status quo that means continued abuse, neglect, pain, and suffering for the nation’s 1.2-million nursing home residents.
LTCCC urges CMS to carefully consider the limitations of the current proposed standard of 3.0 HPRD and the need for a meaningful safe staffing minimum of 4.1 HPRD to improve the lives of nursing home residents.
[1] Bostick JE, Rantz MJ, Flesner MK, Riggs CJ, JAMDA, “Systematic review of studies of staffing and quality in nursing homes,” (April 26, 2006). Available at https://www.jamda.com/article/S1525-8610(06)00051-X/fulltext.
[2] Schnelle, J.F., Simmons, S.F., Harrington, C., Cadogan, M., Garcia, E., & Bates-Jensen, B., “Relationship of nursing home staffing to quality of care,” (2004). Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1361005/.
[3] Harrington C, Kovner C, Mezey M, Kayser-Jones J, Burger S, Mohler M, Burke R, Zimmerman D, The Gerontologist, “Experts Recommend Minimum Nurse Staffing Standards for Nursing Facilities in the United States,” (February 2000). Available at https://pubmed.ncbi.nlm.nih.gov/10750309/.
[4] Harrington C, Ross L, Chapman S, Halifax E, Spurlock B, Bakerjian D, Policy, Politics, & Nursing Practice, “Nurse Staffing and Coronavirus Infections in California Nursing Homes,” (July 7, 2020). Available at https://journals.sagepub.com/doi/10.1177/1527154420938707.
[5] Li Y, Temkin-Greener H, Shan G, and Cai X, Journal of the American Geriatrics Society, “COVID-19 Infections and Deaths among Connecticut Nursing Home Residents: Facility Correlates,” (June 18, 2020). Available at https://agsjournals.onlinelibrary.wiley.com/doi/epdf/10.1111/jgs.16689.
[6] Schnelle, JF, Simmons, SF, Harrington, C, Cadogan, M, Garcia, E, Bates-Jensen, B “Relationship of nursing home staffing to quality of care,” (2004). Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1361005/.
[7] The Nursing Home Reform Act passed into law as part of H.R.3545 – Omnibus Budget Reconciliation Act of 1987. On 12/22/1987 it became Public Law No: 100-203. Available at https://www.congress.gov/bill/100th-congress/house-bill/3545/text. Henceforth, “Nursing Home Reform Law” or “Reform Law.”
[8] 42 CFR § 483.35.
[9] Centers for Medicare & Medicaid Services, Abt Associates Inc., “Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes. Report to Congress: Phase II Final,” (2001). Available at https://theconsumervoice.org/uploads/files/issues/CMS-Staffing-Study-Phase-II.pdf.
[10] The White House, “FACT SHEET: Protecting Seniors by Improving Safety and Quality of Care in the Nation’s Nursing Homes,” (February 28, 2022). Available at https://www.whitehouse.gov/briefing-room/statements-releases/2022/02/28/fact-sheet-protecting-seniors-and-people-with-disabilities-by-improving-safety-and-quality-of-care-in-the-nations-nursing-homes/.
[11] Centers for Medicare & Medicaid Services, Abt Associates, “Nursing Home Staffing Study Comprehensive Report,” (June 2023). Available at https://www.cms.gov/files/document/nursing-home-staffing-study-final-report-appendix-june-2023.pdf.
[12] Centers for Medicare & Medicaid Services, “Centers for Medicare & Medicaid Services Staffing Study to Inform Minimum Staffing Requirements for Nursing Homes,” (August 22, 2022). Available at https://www.cms.gov/blog/centers-medicare-medicaid-services-staffing-study-inform-minimum-staffing-requirements-nursing-homes.
[13] “Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes,” available at www.nursinghome411.org/staffing.
[14] Harrington, C., Kovner, C., Mezey, M., Kayser-Jones, J., Burger, S., Mohler, M., Burke, B., and Zimmerman, D. “Experts Recommend Minimum Nurse Staffing Standards for Nursing Facilities in the U.S.,” (February 2000). Available at https://pubmed.ncbi.nlm.nih.gov/10750309/.
[15] LTCCC, “24-Hour Registered Nurses in Nursing Homes: Affordable, Attainable, & Necessary,” (September 27, 2023). Available at https://nursinghome411.org/costs-24-hour-rn/.
[16] Chen MM, Grabowski DC, Health Economics, “Intended and Unintended Consequences of Minimum Staffing Standards for Nursing Homes, (May 22, 2014). Available at https://onlinelibrary.wiley.com/doi/10.1002/hec.3063
[17] Bowblis JR, Health Serv Res., “Staffing ratios and quality: an analysis of minimum direct care staffing requirements for nursing homes,” (October 2011). Available at https://pubmed.ncbi.nlm.nih.gov/21609329/.
[18] See expert comments (Charlene Harrington, et al.), p. 50. Available at https://www.regulations.gov/comment/CMS-2023-0144-9587.
[19] In California and Ohio, the implementation of minimum staffing requirements coincided with a five percent increase in HPRD overall. Though the regulations unintentionally resulted in a reduction in skill mix (i.e., the ratio of RNs to all direct care staff), the staffing requirements led to a decrease in severe deficiency citations and improvement in specific health conditions requiring intensive nursing care. See Chen MM, Grabowski DC, Health Economics, “Intended and Unintended Consequences of Minimum Staffing Standards for Nursing Homes, (May 22, 2014). Available at https://onlinelibrary.wiley.com/doi/10.1002/hec.3063.
[20] CMS’s 2001 study established the importance of having a minimum of 0.75 RN HPRD, 0.55 LPN/LVN HPRD, and 2.8 (to 3.0) CNA HPRD, for a total of 4.1 nursing HPRD.
[21] Hawk T, White EM, Bishnoi C, Schwartz LB, Baier RR, Gifford DR, “Facility characteristics and costs associated with meeting proposed minimum staffing levels in nursing homes,” (2022). Available at https://pubmed.ncbi.nlm.nih.gov/35113449/.
[22] See expert comments (Charlene Harrington, et al.), page 14. Available at https://www.regulations.gov/comment/CMS-2023-0144-9587.
[23] Nursing homes in New York are required to maintain daily minimum staffing hours equal to 3.5 hours of care per resident per day by a CNA, LPN, or RN. New York State issues a notice of noncompliance using CMS’s PBJ data when a facility fails to meet the minimum staffing standard. See New York Nursing Home Minimum Staffing and Direct Resident Care Spending. Available at https://www.health.ny.gov/facilities/nursing/minimum_staffing/#:~:text=Nursing%20Homes%20are%20required%20by,practical%20nurse%2C%20or%20registered%20nurse.
[24] U.S. Senate Special Committee on Aging, “Uninspected and Neglected: Nursing Home Inspection Agencies are Severely Understaffed, Putting Residents at Risk,” (May 2023). Available at https://www.aging.senate.gov/imo/media/doc/UNINSPECTED%20&%20NEGLECTED%20-%20FINAL%20REPORT.pdf.
[25] LTCCC, “Broken Promises: An assessment of federal data on nursing home oversight and the impact of lax enforcement on residents and families,” (2021). Available at https://nursinghome411.org/wp-content/uploads/2021/10/Broken-Promises.NH-Oversight-Data-Assessment.pdf.
[26] LTCCC, “Broken Promises: An Assessment of Nursing Home Oversight,” (November 2021). Available at https://nursinghome411.org/reports/survey-enforcement/survey-data-report/.
[27] See LTCCC’s Elder Justice “No Harm” Newsletter, (Volume 3, Issue 8). Available at https://nursinghome411.org/elder-justice-3-8/.
[28] Edelman T, Center for Medicare Advocacy, “Report: Nursing Staffing Deficiencies,” (January 10, 2019). Available at https://medicareadvocacy.org/report-nurse-staffing-deficiencies/.
[29] Braun RT, Jung H, Casalino LP, Myslinski Z, and Unruh MA, JAMA Health Forum, “Association of Private Equity Investment in US Nursing Homes With the Quality and Cost of Care for Long-Stay Residents,” (November 19, 2021). Available at https://jamanetwork.com/journals/jama-health-forum/fullarticle/2786442. Gupta A, Howell ST, Yannelis C, and Gupta A, National Bureau of Economic Research, “Does Private Equity Investment in Healthcare Benefit Patients? Evidence from Nursing Homes,” (February 2021). Available at https://www.nber.org/papers/w28474.
[30] Department of Health and Human Services Office of Inspector General, “Adverse Events in Skilled Nursing Facilities: National Incidence Among Medicare Beneficiaries, (February 2014). Available at https://oig.hhs.gov/oei/reports/oei-06-11-00370.pdf.
[31] Harrington C, Montgomery A, King T, Grabowski DC, and Wasserman M, Health Affairs, “These Administrative Actions Would Improve Nursing Home Ownership and Financial Transparency In The Post COVID-19 Period,” (February 11, 2021). Available at https://www.healthaffairs.org/do/10.1377/forefront.20210208.597573/.
[32] Telvock D, Moretti, L, “Nursing home industry says ‘the staff are not there’ to meet federal staffing plan,” (October 30, 2023). Available at https://www.wivb.com/news/nursing-home-industry-says-the-staff-are-not-there-to-meet-federal-staffing-plan/.
[33] Centers for Medicare & Medicaid Services, Provider Information. Available at https://data.cms.gov/provider-data/dataset/4pq5-n9py.
[34] White, E. M., Aiken, L. H., & McHugh, M. D., “Registered nurse burnout, job dissatisfaction, and missed care in nursing homes,” (October 2019). Available at https://pubmed.ncbi.nlm.nih.gov/31334567/.
[35] PHI, “Direct Care Workers in the United States,” (2022). Available at https://www.phinational.org/wp-content/uploads/2022/08/DCW-in-the-United-States-2022-PHI.pdf
[36] Berridge C, Lima J, Schwartz M, Bishop C, and Miller SC, JAMDA, “Leadership, Staff Empowerment, and the Retention of Nursing Assistants: Findings from a Survey of U.S. Nursing Homes,” (September 2020). Available at https://www.jamda.com/article/S1525-8610(20)30147-X/fulltext.
[37] 42 U.S.C. § 1320a–5. Available at https://www.govinfo.gov/app/details/USCODE-1995-title42/USCODE-1995-title42-chap6-subchapXI_2-partA-sec1320a-5/summary.
[38] See LTCCC’s policy brief, “LTC Medicaid Funding: Separating Fact from Fiction,” (Updated September 2023). Available at https://nursinghome411.org/ltc-medicaid-funding/.
[39] Hawk T, White EM, Bishnoi C, Schwartz LB, Baier RR, Gifford DR, “Facility characteristics and costs associated with meeting proposed minimum staffing levels in nursing homes,” (April 2022). Available at https://pubmed.ncbi.nlm.nih.gov/35113449/.
[40] MACPAC, “Principles for Assessing Medicaid Nursing Facility Payment Policies, Chapter 2,” (March 2023). Available at https://www.macpac.gov/wp-content/uploads/2023/03/Chapter-2-Principles-for-Assessing-Medicaid-Nursing-Facility-Payment-Policies.pdf.
[41] MedPAC, “Skilled Nursing Facility Services Payment System,” (Revised October 2023). Available at https://www.medpac.gov/wp-content/uploads/2022/10/MedPAC_Payment_Basics_23_SNF_FINAL_SEC.pdf.
[42] Harrington, C., Montgomery, A., King, T., Grabowski, D., and Wasserman, M., Health Affairs Forefront, “These Administrative Actions Would Improve Nursing Home Ownership and Financial Transparency in the Post COVID-19 Period,” (February 11, 2021). Available at https://www.healthaffairs.org/do/10.1377/forefront.20210208.597573/full.
[43] Manatt, “Recommendations to Strengthen the Resilience of New Jersey’s Nursing Homes in the Wake of COVID19,” (June 2, 2020). Available at https://manatt.com/Manatt/media/Documents/NJ-LTC-Report.pdf.
[44] Jaffe S, “3 States Limit Nursing Home Profits in Bid to Improve Care,” (October 25, 2021). Available at https://kffhealthnews.org/news/article/3-states-limit-nursing-home-profits-in-bid-to-improve-care/.
[45] P.L. 2020, c. 89. Available at https://www.njleg.state.nj.us/Bills/2020/PL20/89_.PDF.
