February 13, 2024 – Nursing home residents are among the most vulnerable members of our society. However, the nursing homes in which they live are often riddled with neglect, abuse, and substandard care. Addressing these issues is paramount for ensuring that nursing home residents receive the highest standards of care and support they need.
The Long Term Care Community Coalition brings these issues to light in our publications of the Senior Care Policy Briefing and the Elder Justice Newsletter, available on NursingHome411 and via email updates.
The Senior Care Policy Briefing, a concise, bi-monthly one-page newsletter, is committed to keeping stakeholders abreast of the most recent policy developments influencing long-term care. We track regulatory shifts, legislative updates, news articles, and scholarly research to spotlight incongruities between the provider industry’s public narrative depicting financial challenges and its notably optimistic financial reports to stakeholders. Our overarching aim is to offer an insightful reality check on industry assertions regarding funding sufficiency, staffing concerns, and other pertinent issues.
The Elder Justice Newsletter, published with the Center for Medicare Advocacy, provides examples of health violations in which surveyors identified neither harm nor immediate jeopardy to resident health, safety, or well-being. The newsletter aims to provide readers with real stories of resident pain, suffering, and humiliation from across the country, so that readers can judge for themselves whether a violation was “no harm.” The examples are taken directly from Statement of Deficiencies (SoDs) on CMS’s Care Compare (formerly Nursing Home Compare) website. You can find a user-friendly guide featuring the Elder Justice Newsletters published in 2023 (and prior!) that details the “no harm” deficiencies we’ve covered. Users can sort the guide by F-Tag, provider name, CMS star rating, state, city, and zip code.
Together, LTCCC’s newsletters provide an uncompromising overview of critical issues in elder care, from specific instances of deficiencies to broader policy considerations. Sign up to receive the Senior Care Policy Briefing and Elder Justice Newsletter in your inbox.
Excerpt from the Senior Care Policy Briefing:
Read the full briefing at https://nursinghome411.org/policybriefing-dec28/.
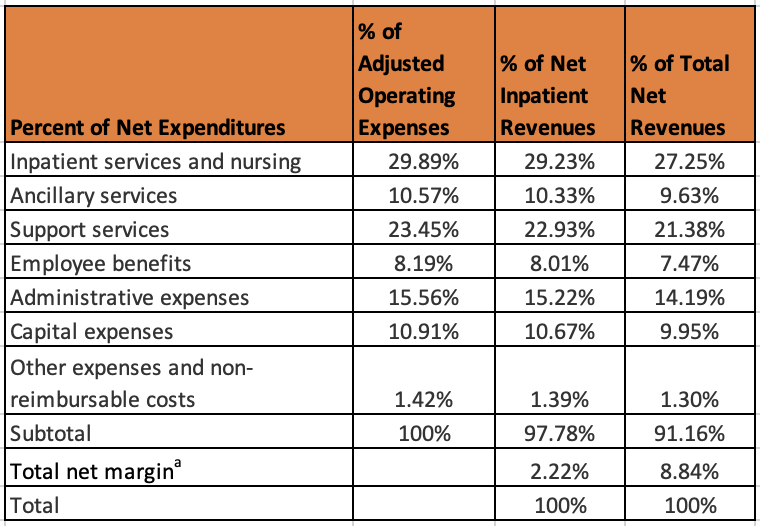
A new national study of nursing home profits and finances found that, when disallowed costs and non-cash depreciation expenses are excluded, the average nursing home profit margin is close to 9%. The study, co-authored by LTCCC’s Executive Director Richard Mollot, with support from FJC – A Foundation of Philanthropic Funds, assessed facility cost reports for the year 2019. Its findings underscore the importance of improving accountability for the use of the public funds which pay for the majority of nursing home care.
Other key findings from the study include:
- Not counting profits from disallowed costs and non-cash depreciation, nursing homes reported total net revenues of $126 billion and a profit of $730 million (0.58%) in 2019.
- Approximately 77% of nursing homes reported making over $11 billion in payments to related parties.
- Overall spending for direct care was 66% of net revenues, including 27% on nursing, in contrast to 34% spent on administration, capital, other, and profits.
Example from the Elder Justice Newsletter:
Read the full newsletter at https://nursinghome411.org/elder-justice-5-1/.
Improper diagnosis: Resident receives antipsychotic without clinical indication for its use.
- In this deficiency, a nursing home resident received an unnecessary antipsychotic medication, lacking clinical justification. The resident’s diagnoses included Alzheimer’s, depression, and anxiety, and the resident was prescribed a medication for generalized anxiety disorder in May 2022. Subsequent months revealed no documented behavioral issues, and the director of nursing stated in August 2022 that the resident lacked both behavioral problems and a proper diagnosis for the prescribed medication. Though psychotropic drugs should not be administered unless necessary to treat a specific condition as diagnosed and documented in the resident’s clinical record, the surveyor cited the violation as no harm.
Federal data indicate that most health violations (more than 95%) are cited as causing “no harm” to residents. The failure to recognize resident pain, suffering, and humiliation when it occurs too often means nursing homes are not being held accountable.
–Broken Promises: An Assessment of Nursing Home Oversight
What is a “No Harm” deficiency? Nursing homes voluntarily participating in the Medicare and Medicaid programs agree (and are paid) to adhere to minimum standards of care established by the federal Nursing Home Reform Law and its implementing regulations. These standards exist to ensure that every nursing home resident is provided services that help attain and maintain their “highest practicable physical, mental, and psychosocial well-being.” Under the Reform Law, nursing homes that fail to meet the federal requirements are subject to various penalties, based on the scope and severity of the violation(s).
To receive the Elder Justice Newsletter and Senior Care Policy Briefing, please sign up for LTCCC alerts at https://nursinghome411.org/join/.
