The Senior Care Policy Briefing covers important long-term care issues by highlighting policy updates, news reports, and academic research.
Read the full Senior Care Policy Briefing below or download here.
April 30, 2025.
NEWSFLASH
- A groundbreaking lawsuit filed by Maryland nursing home residents has been cleared to proceed by a federal judge. The residents claim the state’s Department of Health violated their rights under the Americans with Disabilities Act by failing to conduct routine inspections and properly oversee nursing home care. (The case is being led by the Public Justice Center and Justice in Aging.)
- According to the complaint, many facilities went years without inspections, leading to serious issues such as pressure ulcers, falls, and infections. Some residents were confined to their beds or rooms for months without proper care. At the time the lawsuit was filed, some nursing homes hadn’t been inspected in up to four years.
- The residents argue that regular inspections could have identified and addressed these dangers. Maryland, like many states, is struggling with a severe backlog worsened by the COVID-19 pandemic. A 2023 U.S. Senate investigation found that nationwide, one in nine nursing homes had not been inspected in at least two years. Maryland’s inspection delays date back decades.
“Plaintiffs allege that they are harmed by [Maryland Department of Health’s] “delayed complaint investigations” that often result in findings of no violations “due only to difficulties locating documents, staff turnover, or the subsequent discharge or death of the resident.””
PRIVATE EQUITY, PUBLIC RISK
- New findings from the Private Equity Stakeholder Project reveal that private equity (PE) firms continue to acquire nursing homes, often at the expense of resident care. Despite industry claims that private investment is declining, PE may now own as much as 13% of U.S. nursing homes—significantly higher than the widely cited 5% estimate.
- The report calls for stronger oversight, including better ownership reporting, tighter review of nursing home sales, bans on risky financial practices, and improved staffing standards. With federal reforms moving slowly, state action is critical to protecting nursing home residents from financial exploitation and declining care.
TURNING PRESSURE ULCERS INTO PROFITS
- The U.S. Department of Justice (DOJ) has filed a False Claims Act case against Vohra Wound Physicians Management, one of the nation’s largest specialty wound care providers. Vohra contracts with nursing homes across the country to provide wound care services to residents. DOJ allegations include that Vohra “hired physicians without wound care expertise,” set care service “targets based solely on revenue goals,” and submitted “false claims” for services that were not medically necessary.
LAWMAKERS PROBE NURSING HOME FINANCES
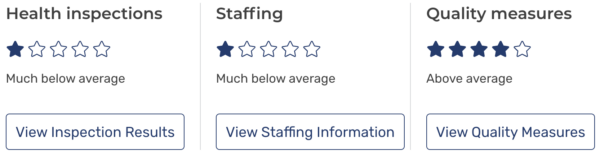
- A CBS 6 investigation uncovered financial irregularities and poor care at Colonial Heights Rehabilitation and Nursing Center, a Virginia nursing home with a 1-star federal rating. Despite claiming losses, the facility shifted millions in profits to related companies through inflated rent payments. Now, lawmakers are calling on CMS to audit the facility and crack down on hidden profits.