The Senior Care Policy Briefing covers important long-term care issues by highlighting policy updates, news reports, and academic research.
Read the full Senior Care Policy Briefing below or download here.
September 15, 2023.
NEWSFLASH
- On September 1, CMS released the long-awaited minimum nursing home staffing proposal, which would require 3.0 hours per resident day (HPRD) of nurse staffing time. Sadly, this is “wholly inadequate to meet the needs of nursing home residents,” due to the fact that it falls far below what numerous studies have found to be the minimum necessary to keep residents safe (no matter treat them humanely or provide effective infection control). In fact, it is far below what CMS identified as the minimum necessary over 20 years ago, a time when residents had fewer needs.
- Experts are observing a rise in COVID-19 cases, indicating a potential late-summer surge that could disproportionately impact nursing homes. The CDC recorded a notable increase in cases among nursing home residents in July, with rising hospitalizations and concerns about a resurgence. Despite a decline in the COVID-19 death rate, experts warn of the possibility of worsening outcomes if hospitalizations continue to climb.
- COVID-19 exacerbated feelings of loneliness among nursing home residents, isolating them from family and social interactions, according to a new report on resident experiences during the pandemic. “It was like a big, sad feeling of being alone came over our residents. They were separated from their families, their routines disrupted,” says lead author Audrieanna Raciti.
LTC BY THE NUMBERS
- While Nursing Homes Cry Poverty to Congress, They Boast of Strong Financials to Investors.
- Omega Healthcare Investors reported strong Q2 financial results driven by improved occupancy rates, higher state reimbursements, and labor market enhancements. The company also made substantial investments in its skilled nursing sector portfolio and expressed confidence in the senior care sector’s overall improvement.
- Pillars of Stability. National Health Investors, a REIT with over 200 senior living facilities across 33 states, reported that its continuing care retirement communities and nursing homes “remain pillars of stability.”
- NHI announced that it will pay its third-quarter dividend of $0.90 per share.
- How Do They Get Away With It? Donations from individuals and PACs associated with hospitals and nursing homes spiked to $111 million in 2020. The industry’s highest previous total was $35 million in 2016.
GET THE FACTS
- In July, CMS instituted enhanced oversight rules for new hospices in several states due to an uptick of fraudulent activity among hospices. CMS also revealed that it would be conducting unannounced site visits to every hospice enrolled in Medicare. As of late August, more than 7,000 hospices were visited.
- “Hospice has come under increasing fire over recent years, initially from reports about hospices that perform poorly on health and safety standards and endanger vulnerable patients, and more recently with respect to dramatic growth in the number of hospice providers in some western states that have raised program integrity concerns.” – William Dombi, president of the National Association for Home Care & Hospice
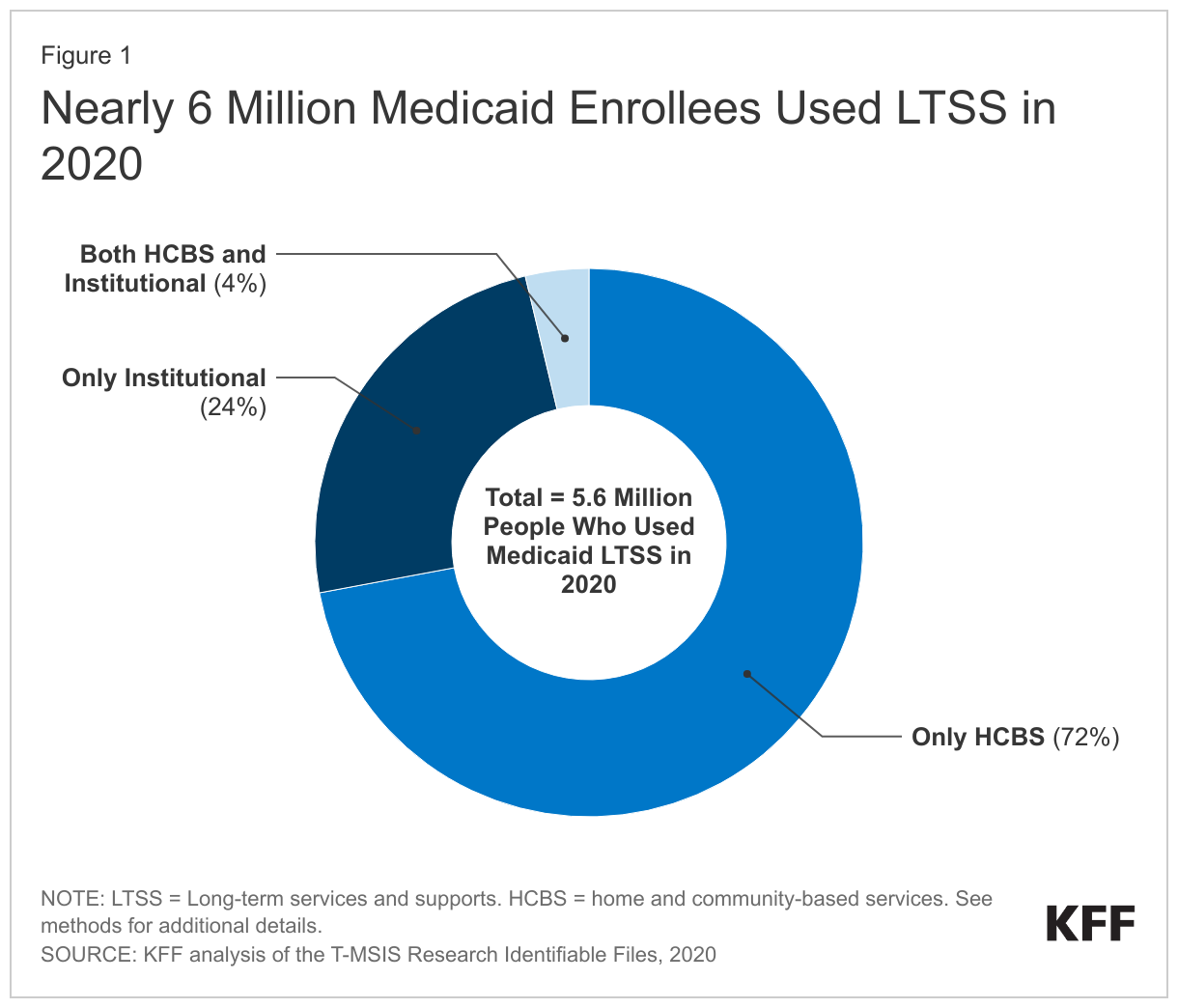
The nursing home industry is claiming that any safe staffing requirement would result in facility closures. However, as shown by the graphic (right) from Kaiser Family Foundation, most people no longer get long-term services and supports (LTSS) in nursing homes. For years, the number of facilities has been decreasing as more Americans seek to avoid nursing home placement and more states shift their Medicaid programs away from institutional nursing homes and toward home and community based services (HCBS).