June 30, 2022 – Surveys (inspections) are the principal mechanism by which the government assesses nursing home quality and determines compliance with standards of care. Unfortunately, as previous LTCCC studies have shown, State Survey Agencies (SAs) – which are charged with monitoring care, responding to complaints, and ensuring compliance with minimum standards – too often fail to ensure that residents are protected from poor care, abuse, and neglect.
To help address these issues, yesterday the Centers for Medicare & Medicaid Services (CMS) released important updates to its surveyor guidance on key areas including infection prevention, staffing, and abuse and neglect.
The following topics are addressed in the revised guidance:
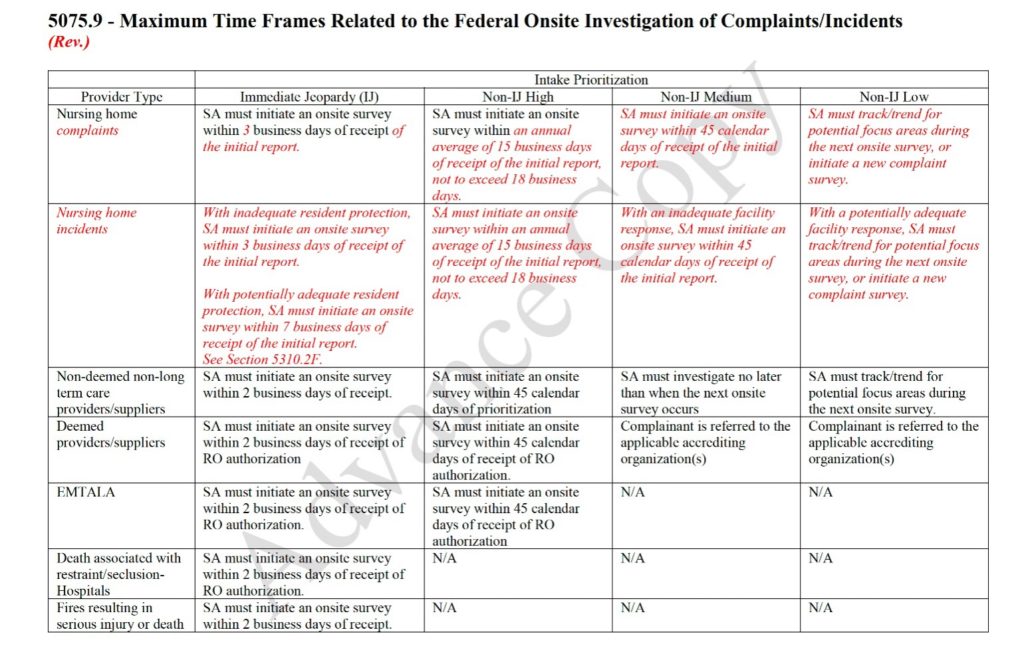
- Investigation of Complaints & Facility-Reported Incidents: Clarifies timeliness of state investigations, and communication to complainants to improve consistency across states. More information on these changes can be found in the chart below and in LTCCC’s Summary of Complaint Handling Requirements.
- Abuse and Neglect: CMS has made significant revisions to the guidance for Abuse/Neglect. CMS is providing clarifications to surveyors about facility reported incidents, including examples of cases and what information should be reported.
- Admission, Transfer, and Discharge: Clarifies requirements related to facility-initiated discharges. Inappropriate and unsafe discharges are a serious and widespread problem.
- Mental Health/Substance Use Disorder (SUD): Improve guidance related to meeting the unique health needs of residents with mental health needs and SUD. CMS clarified that when facilities care for residents with these conditions, policies and practices must not conflict with resident rights or other requirements of participation. Facility staff are expected to have knowledge of signs and symptoms of possible substance use, and be prepared to address emergencies (e.g., an overdose).
- Nurse Staffing (Payroll-Based Journal): Uses payroll-based staffing data to trigger deeper investigations of sufficient staffing. This is important because, even though most nursing homes fail to provide sufficient staff to meet the needs of their residents, they are rarely cited for insufficient staffing and almost never face a fine (even when insufficient staffing leads to harmful or degrading conditions!).
- Resident Rights: New guidance addresses the issue of residents’ rights to safe visitation while adhering to the “core principles” of infection control and prevention.
- Potential Inaccurate Diagnosis and/or Assessment: Addresses situations where practitioners or facilities may have inaccurately diagnosed/coded a resident with schizophrenia in the resident assessment instrument. As The New York Times reported last fall, the “phony” diagnosis of schizophrenia among nursing home residents hides the high rate of dangerous antipsychotic drugging in too many nursing homes.
- Pharmacy: Addresses situations where practitioners or facilities may have inaccurately diagnosed/coded a resident with schizophrenia in the resident assessment instrument.
- Infection Control: Facilities have been required to have an infection preventionist for several years (prior to the COVID-19 pandemic). CMS is strengthening this requirement to better ensure that facilities are effectively mitigating the onset and spread of infections.
- Arbitration: The use of pre-dispute arbitration agreements by nursing homes is a long-standing concern to LTCCC and other resident advocates. Facilities use these agreements, which can be hard for the average person to identify, no matter understand, to prevent a resident or their family from ever suing the facility, no matter how heinous the abuse or neglect. The new guidance prohibits nursing homes from requiring residents to sign binding arbitration agreements as a condition of admission to the facility, or as a requirement to continue to receive care at that facility. The arbitration guidance also addresses other requirements (i.e., allowing residents to choose a neutral arbitrator; facilities making final arbitrator’s decision available for review by CMS or its designee).
- Psychosocial Outcome Severity Guide: The failure to hold nursing homes accountable for psychosocial harm to residents is a longstanding and serious problem. Too many nursing homes treat residents in a demeaning manner, providing services and activities that are based on how much they want to spend on these services, as opposed to meeting their residents’ personal needs and goals (as federal law requires). The new guidance provides greater clarification on how to identify when a resident has suffered psychosocial harm.
Note: LTCCC’s Guide to Nursing Home Oversight & Enforcement identifies key requirements for state agencies in the federal regulatory requirements and the State Operations Manual which lays out detailed expectations and guidance for state surveyors. It is a useful resource for anyone interested in understanding what to expect from the government agencies charged with ensuring nursing home resident safety and dignity. This document will be revised in the near future to reflect recent announced changes.
