The Senior Care Policy Briefing covers important long-term care issues by highlighting policy updates, news reports, and academic research.
Read the full Senior Care Policy Briefing below or download here.
September 30, 2025.
NEWSFLASH
- A new federal investigation by the Department of Health and Human Services (HHS) Office of Inspector General (OIG) reveals that nursing homes failed to report 43% of falls with major injury and hospitalization among Medicare-enrolled residents between July 2022 and June 2023.
-
- Facilities omitted nearly 18,400 of 42,000 such falls from their federally required Minimum Data Set (MDS) assessments.
- For-profit, chain-affiliated, and large nursing homes had the highest rates of underreporting, and reporting varied widely by state, ranging from 21 percent unreported in South Dakota to 64 percent in Washington, DC. Falls were least likely to be reported for younger residents, men, short-stay residents, and those with Medicare-only coverage.
- The OIG emphasized that this widespread underreporting makes CMS’s Care Compare website unreliable, since facilities with the lowest reported fall rates were often the least likely to disclose serious falls.
- Even five-star facilities underreporting nearly half of serious incidents.
- OIG recommended that CMS strengthen validation of nursing home data, use Medicare claims to verify falls, and extend improvements to other quality measures prone to manipulation. CMS concurred and has begun efforts to supplement MDS data with claims, but OIG cautioned that meaningful reforms could take years to implement.
- HHS has asked courts to dismiss appeals defending portions of the 2024 federal nursing home staffing mandate, after judges in Texas and Iowa struck down key requirements such as 24/7 registered nurse coverage and minimum staffing hours.
RESEARCH ROUNDUP
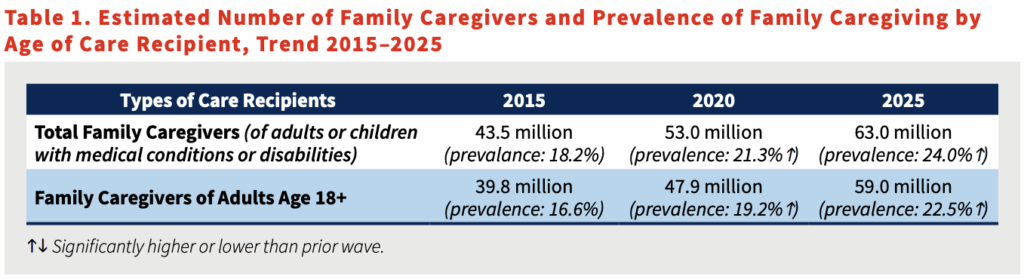
- The new Caregiving in the U.S. 2025 report finds that nearly 63 million adults, about one in four Americans, are providing care to a loved one with illness, disability, or age-related needs. This represents a 45% increase since 2015, underscoring the growing reliance on families to sustain our long-term care system.
- Caregivers provide intensive support, often averaging 27 hours a week, while juggling work, finances, and their own health. Yet most lack training and adequate support.